COMPREHENSIVE GUIDE TO SKIN CANCER
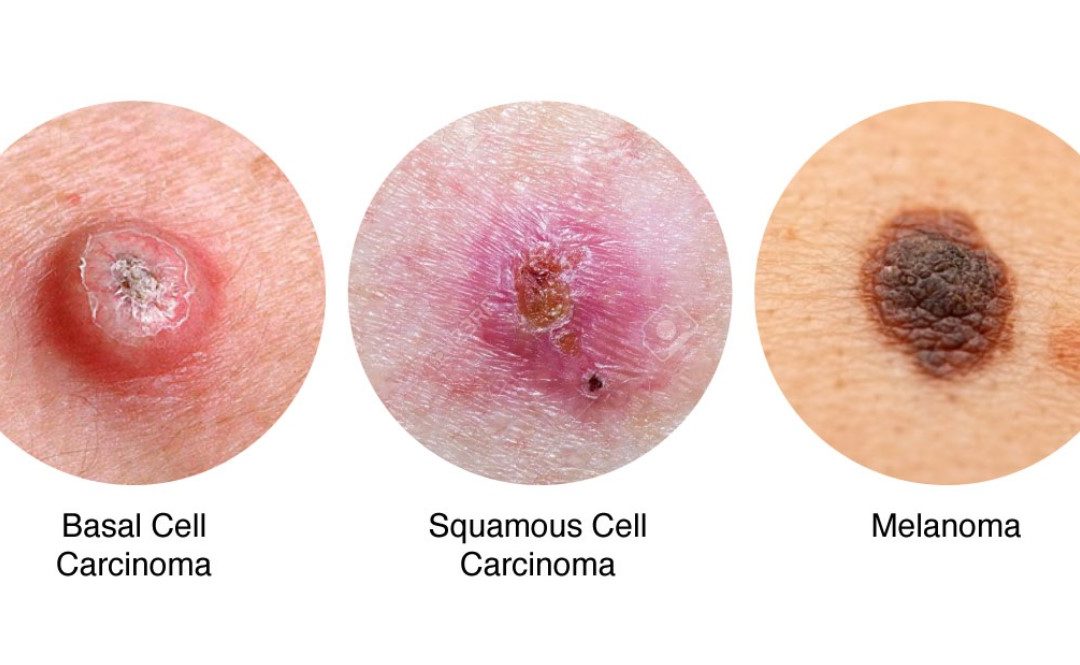
Skin cancer — the abnormal growth of skin cells — most often develops on skin exposed to the sun. But this common form of cancer can also occur on areas of your skin not ordinarily exposed to sunlight. There are three major types of skin cancer — basal cell carcinoma, squamous cell carcinoma and melanoma.
Basal Cell Carcinoma (BCC)
Basal cell carcinoma (BCC) is the most common skin cancer. It is abnormal, uncontrolled lesion that arises in the skin’s basal cells, which line the deepest layer of the epidermis (the outermost layer of the skin).
It presents as sores, red patches, pink growths, shiny bumps, or scars and is usually caused by a combination of cumulative and intense, occasional sun exposure. BCC almost never spreads (metastasizes) beyond the original tumour site.
What are the clinical features of BCC?
BCC can vary in their appearance, but most usually it appears as:
- Slowly growing plaque or nodule. Sometimes the patch crusts
- May be skin coloured, pink or pigmented
- Pink growth with elevated rolled border, crusted indentation in the centre and tiny vessels on the surface
- Can bleed and ooze
- Can present as a scar-like area
- May ulcerate
- Vary in size from few millimetres to several centimetres in diameter
- In addition to the signs of BCC listed above, any change in a preexisting skin growth, such as an open sore that fails to heal, or the development of a new growth, should prompt an immediate review
Squamous Cell Carcinoma (SCC)
Squamous cell carcinoma (SCC) is the second most common skin cancer. It is sometimes called cutaneous squamous cell carcinoma (cSCC) to differentiate it from very different kinds of SCCs elsewhere in the body.
It can often appear as a firm pink lump with a rough or crusted surface. It is more common on sun exposed areas such as the head, ears, neck and back of the hands. It can metastasize elsewhere and must be treated early. 1 in every 770 New Zealanders develops SCC each year.
What are the clinical features of cSCC?
SCC can vary in their appearance, but most usually it appears as:
- Scaly or crusty raised area of skin with a red, inflamed base
- Hard plaque or a papule
- May look like warts
- May be painful or tender
- Can bleed, especially from the lip
- May ulcerate
- Grows over weeks or months
- Vary in size from few millimetres to several centimetres in diameter
- In addition to the signs of SCC listed above, any change in a pre-existing skin growth, such as an open sore that fails to heal, or the development of a new growth, should prompt an immediate review
Malignant Melanoma (MM)
Melanoma is a malignant tumour of melanocytes. Melanocytes are cells that produce the dark pigment, melanin, which is responsible for the color of skin. Melanoma is described as:
- in situ, if the tumour is confined to the epidermis
- Invasive, if the tumour has spread into the dermis
- Metastatic, if the tumour has spread to other tissues
What are the clinical features of MM?
MM can vary in the appearance, but most usually it appears as:
- Unusual looking freckle or mole
- Variety of colours, including no pigment
- Can be flat or raised
- Can be itchy or tender
- New mole or an existing one that is growing, changing colour (either becoming lighter or darker) or becoming irregular in some way
What are the risk factors for BCC and SCC?
The main risks factors for developing cSCC are:
- Cumulative sun exposure
- Older age
- Gender-more common in male patients
- Fair skin, blue or green eyes, blond or red hair
- Previous skin cancer
- Actinic keratosis
- Ionizing radiation
- Immunosuppression
- Chronic inflammation
- Scars & chronic wound (Marjolin’s ulcer)
- Chemical-arsenic exposure, smoking, hydrocarbons
- Family history
What are the risk factors for malignant melanoma?
The main risks factors for developing MM are:
- Cumulative sun exposure
- Older age
- Previous invasive MM
- Previous non-melanoma skin cancer (BCC, SCC)
- Many melanocytic naevi (moles)
- Multiple (>5) atypical naevi
- Strong family history of melanoma with 2 or more first-degree relatives affected
- Tanning beds
- Genetic risk factors-BRAF and p53 mutation
How are skin cancers diagnosed?
To diagnose skin cancer, your doctor may:
- Examine your skin. Your doctor may look at your skin to determine whether your skin changes are likely to be skin cancer. Further testing may be needed to confirm that diagnosis
- Remove a sample of suspicious skin for testing (skin biopsy). Your doctor may remove the suspicious-looking skin for lab testing. A biopsy can determine whether you have skin cancer and, if so, what type of skin cancer you have.
When to see a doctor?
Make an appointment with the skin cancer specialist if you notice any changes to your skin that worry you. Not all skin changes are caused by skin cancer. Dr Mackenzie will investigate your skin changes to determine a cause.
Recent Comments