TRIGGER FINGER: DIAGNOSIS AND TREATMENT FOR QUICK RELIEF
Trigger finger or thumb is a condition that causes pain, stiffness, and a sensation of locking or catching when you bend and straighten your finger. The condition is also known as “stenosing tenosynovitis.” Trigger finger or thumb is caused by a thickening around the tendon which bends your finger or thumb. The ring finger and thumb are most often affected by trigger finger, but it can occur in the other fingers, as well. It is more common in women than men and may be linked to diabetes.
Treatment is needed if the triggering of your finger or thumb is causing discomfort or stopping you from being able to perform normal daily activities.
What are the symptoms of trigger finger/thumb?
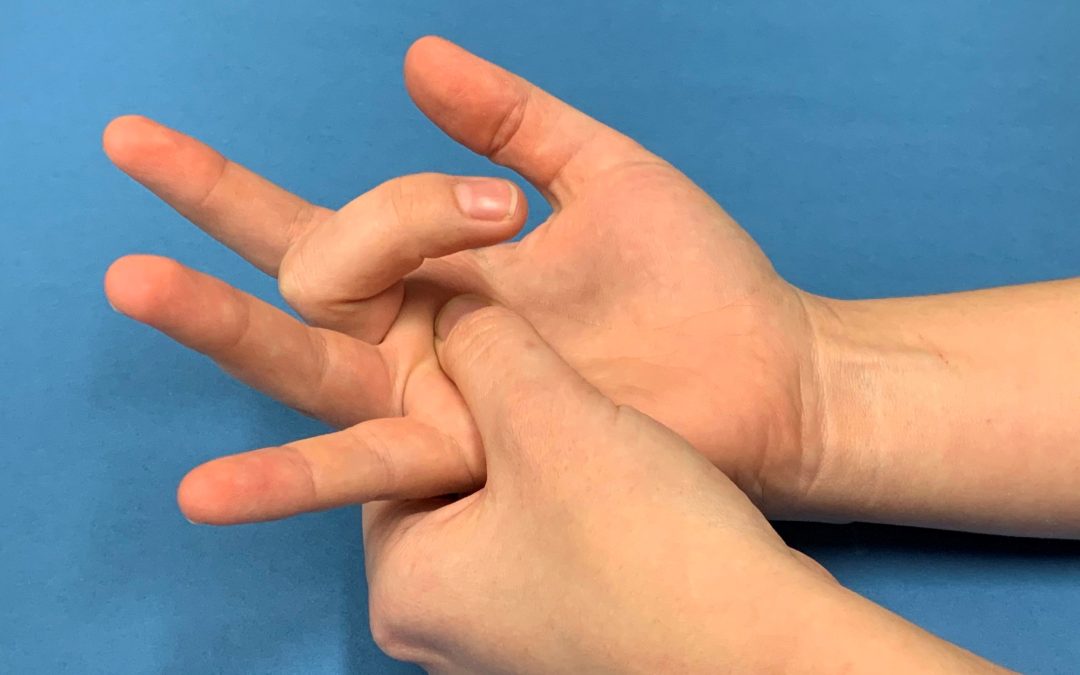
Symptoms of trigger finger/thumb often start without a single injury. They may follow a period of heavy or extensive hand use, particularly pinching and grasping activities. They may include:
- Swelling, stiffness and pain with the grasp
- Tender lump at the base of the finger/thumb on the palm side of the hand
- Catching or locking sensation with finger movement
- Pain on bending or straightening of the finger
- In severe cases, involved finger may become locked in a bent position
- May develop following carpal tunnel decompression
How is trigger finger/thumb diagnosed?
Dr Mackenzie will take a detailed history including complete medical history, how the hands have been used, and any prior injuries.
That will be followed by examination of the hand. Dr Mackenzie will check the finger for stiffness, signs of locking, tenderness over the flexor sheath in the palm and thickening of the tendon. Diagnosis of triggering may need to be made by injection of lignocaine into the flexor sheath to unlock the digit.
Why do I need surgery?
Trigger finger and trigger thumb are not harmful but can be a painful nuisance. If your symptoms are constant, don’t recover over a few weeks without treatment and are not relieved by non-surgical measures, surgery may be needed.
What is the treatment?
Non-surgical treatment
Non-surgical treatments are usually tried first. Treatment begins with:
- Wrist splint at night to keep the affected finger or thumb in a straight position while you sleep. A splint can be fitted by a hand therapist
- Resting your hand and avoiding activities that make it worse
- Taking nonsteroidal anti-inflammatory drugs, such as ibuprofen, to relieve pain and inflammation
- Gentle stretching exercises can help decrease stiffness and improve range of motion in the involved digit
- Cortisone can be injected into the tendon sheath at the base of the trigger finger. A steroid injection may resolve the triggering over a period of one day to several weeks in 50-70% of cases. The risks of injection are small, but it very occasionally causes thinning or colour change in the skin at the site of injection, infection. If symptoms do not improve with time, a second injection may be given. If two injections do not help the problem, surgery may be considered. These are less effective in diabetic patients and blood glucose may be more variable and difficult to control for the next few weeks
Surgical treatment
When symptoms are severe or do not improve, surgery may be needed. The decision for surgery is based on how much pain or loss of function you have in your finger. If the finger or thumb is stuck in a flexed position, surgery is recommended to prevent permanent stiffness.
The goal of surgery is to release the A1 pulley that is blocking tendon movement, so the flexor tendon can glide more easily through the tendon sheath.
What happens during surgery?
Triger finger release is done as a day case. The surgery can be done under regional anaesthesia, which numbs up your arm, or under local anaesthesia, which numbs just your hand. In some cases, you will also be given a light sedative through an intravenous line inserted into a vein in your arm.
Dr Mackenzie will make a small incision at the base of the finger to release the pulley causing problems with tendon glide. During the procedure Dr Mackenzie will cut through the A1 pulley to release it and will check that tendon and the finger move smoothly. In severe cases or rheumatoid arthritis, a slip of tendon may need to be cut out. Dr Mackenzie will protect the digital nerves. Wound will be closed and bulky dressing applied.
The surgery takes about 30 minutes.
Recent Comments